
In this article, the author shares his experience with different validation models. The validation is widely accepted in the life sciences industry and follows a lifecycle model. What is not always clear is the specific model or models, to follow and how to navigate through those models in the real world or in other words, the specific deliverables that makes right model, and how those deliverables change during the various interactions along the validation journey.
Drawing on my experience in the validation field, It proposes that organizations follow a dynamic validation model that can support the efficient and optimal operation of their Commissioning, Qualification, and Validation (CQV) program.
Other related terms such as building commissioning (Cx), C&Q, Q&V, and process validation suggest additional or sub-models within the larger proposed CQV operational model. However, based on the experience it has found that they are often loosely defined and even used interchangeably.
The uses, advantages, and drawbacks of these models and their applicability to each of the five elements subjected to validation are facilities, utilities, systems, equipment, and processes, and it need to be understood to determine the right validation model in any given situation. The wider proposed CQV Operational Lifecycle Model is best understood within the context of regulatory expectations and best industry practices.
The following analysis explores well-known validation models, how they fit into a CQV program and observed best practices to support and enhance these models.
Validation Models
The most common validation models in the biopharmaceutical industry are:
● The V-model3
● The W-model4
● Risk-based models for C&Q:
o ASTM-E2500 (2007)5
o ISPE’s Science & Risk-based C&Q Model (2019)6
● FDA’s Process Validation Model (2011)1
The V-Model
Since its appearance in 1994 as a model for system (software) development lifecycle (SDLC)3 [3] and its subsequent adaptation for equipment qualification in 20017, the V-model continues to be a constant reference in validation literature and across many CQV programs.
One side of the V sets the specifications while the other side refers to the testing conducted against those specifications to formally qualify the equipment or system. The bottom of the V is where the equipment or system is built.
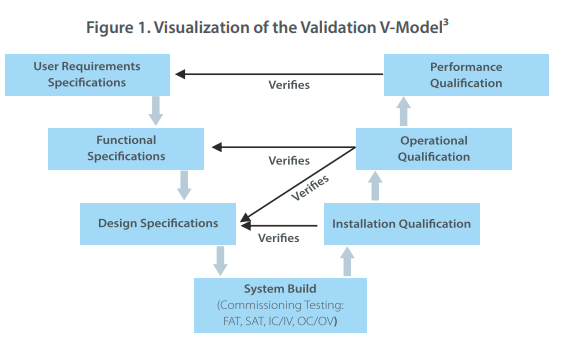 Implicitly embedded in this model is the commissioning testing, which has traditionally been conducted in the form of Factory Acceptance Tests (FAT) and Site Acceptance Tests (SAT)3. Depending on the system and the involvement from the vendor, these standard tests may be supplemented, or replaced, by additional on-site testing. These tests, as per my own experience and industry best practices, include Installation Commissioning (IC) or Installation Verification (IV), followed by Operational Commissioning (OC) or Operational Verification (OV).
Implicitly embedded in this model is the commissioning testing, which has traditionally been conducted in the form of Factory Acceptance Tests (FAT) and Site Acceptance Tests (SAT)3. Depending on the system and the involvement from the vendor, these standard tests may be supplemented, or replaced, by additional on-site testing. These tests, as per my own experience and industry best practices, include Installation Commissioning (IC) or Installation Verification (IV), followed by Operational Commissioning (OC) or Operational Verification (OV).
The primary criticism aimed at this model revolves around its omission of scientific principles and risk-based elements5,6. Particularly, the V-model does not address the essential elements of product and process understanding, which are integral to enhancing the specification aspect of the V. Moreover, it fails to incorporate options for streamlining the testing process through Risk Assessments. Essentially, it lacks illustration of the connections with ICH Q98 and ICH Q89. Nevertheless, based on the experience, the V-model still holds relevance as a foundational framework for CQV requirements.
The “W-Model”
 Although not set up as a risk-based model, my analysis indicates that the “W-model”4 paved the way for subsequent models that use Quality Risk Management (QRM) to simplify the qualification efforts by bringing the commissioning elements outside of the “System Build” box in the V-Model, and explicitly representing the “C-elements” as a center portion within the original V-model.
Although not set up as a risk-based model, my analysis indicates that the “W-model”4 paved the way for subsequent models that use Quality Risk Management (QRM) to simplify the qualification efforts by bringing the commissioning elements outside of the “System Build” box in the V-Model, and explicitly representing the “C-elements” as a center portion within the original V-model.
In this analysis, the “W-Model” added more granularity to what was later identified as “verification testing”. Here I refer to both commissioning testing (e.g., FAT, SAT) and qualification testing (i.e., IQ, OQ, PQ).
Risk-based Models for C&Q
Between 2004 and 2009 the concept of Quality Risk Management (QRM) was highly publicized and promoted by the Food and Drug Administration (FDA)10 and the International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use (ICH Q98 ). This, together increased awareness about product and process understanding, also promoted by ICH (ICH Q89 ), led to the first official risk-based validation model. It was introduced as a standard in 2007 by the American Society for Testing and Materials5 and identified as “The Specification, Design, and Verification Process.”
During discussions about this model, there have been some observations that it involves less granularity of testing; in other words, call “verification” and removing all references to both commissioning or qualification. 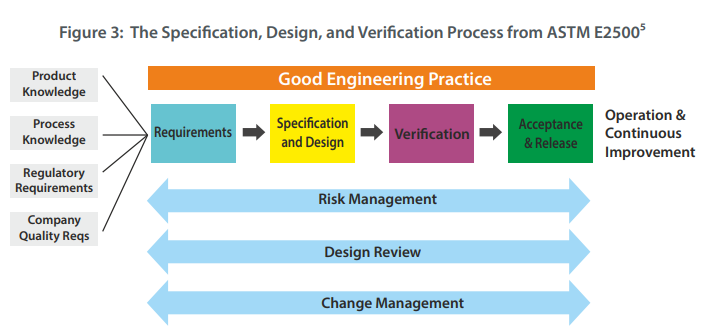 In general, however, my experience with validations is that the benefits far outweigh any of its potential drawbacks, since it allows for more agile navigation through the validation journey by introducing Risk Management and by emphasizing the presence and involvement of subject matter experts with product and process knowledge, balanced with adherence to regulatory requirements and the company’s own quality procedures [5].
In general, however, my experience with validations is that the benefits far outweigh any of its potential drawbacks, since it allows for more agile navigation through the validation journey by introducing Risk Management and by emphasizing the presence and involvement of subject matter experts with product and process knowledge, balanced with adherence to regulatory requirements and the company’s own quality procedures [5].
Model supports leveraging vendor qualification packages and applying traditional commissioning testing, such as FAT and SAT tests, to the qualification phase.
In 2019, the International Society for Pharmaceutical Engineering (ISPE) published a revised version of its Baseline Guide for Commissioning and Qualification6. The guideline in this model replaces the V-model with an integrated commissioning and qualification (C&Q) model that relies on having SMEs from the engineering and equipment side work, alongside other experts from regulatory and quality to establish the user requirements.
Once the initial requirements are established, each facility, utility, system, and equipment are classified as having either a direct or non-direct impact on product quality. The model calls for an improved QRM process that feeds into a Design Review/Design Qualification process iteratively.
The 2019 ISPE Baseline Guide provides more granularity regarding the type and extent of the
verification testing while paving the way for full integration between commissioning deliverables like FAT and SAT with IQ and OQ
The Process Validation Lifecycle
In 2011, the FDA published “Guidance for Industry: Process Validation: General Principles and Practice”1. In this guidance, the FDA adopted a lifecycle approach, moving from process qualification to validation in three stages:
- Stage 1 – Process Design: In this stage the commercial manufacturing process is defined based on knowledge gained through development and scale-up activities.
- Stage 2 – Process Qualification: In this stage the process design is evaluated to determine if the process is capable of reproducible commercial manufacturing. There are two “sub-stages” or “elements”:
- Design of the facility and qualification of the equipment and utilities – This element refers to all C&Q activities applied to the facilities, utilities, systems, and equipment
- Process Performance Qualification (PPQ) – This element refers to the traditional “three successful/successive batches for Process Validation”
- Stage 3 – Continued Process Verification (CPV): There is ongoing assurance that the process remains in a state of control during routine production. This includes routine monitoring of process parameters, trending of data, change control, retraining, and corrective and preventive actions (CAPA), in addition to the periodic review of maintenance and calibration records at pre-established frequencies (e.g., based on risk and system classification). For sterile product manufacturing operations, the annual requalification of critical systems (e.g., autoclaves, SIP) and semi-annual revalidation/re-execution of aseptic process simulations (i.e., media fill program) is also part of this Stage 3 CPV.
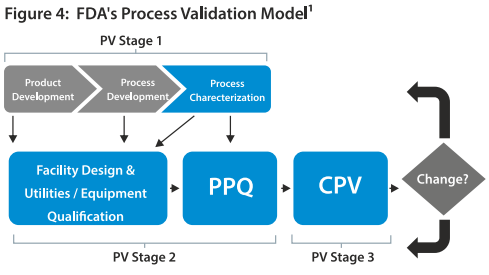 Four years later, in 2015, “Annex 15: Qualification & Validation” was published as part of the EU Guidelines for Good Manufacturing Practice for Medicinal Products for Human and Veterinary Use2. The following year, EMA published two process validation guidelines11,12. These guidelines used a similar lifecycle approach to the one used by the FDA.
Four years later, in 2015, “Annex 15: Qualification & Validation” was published as part of the EU Guidelines for Good Manufacturing Practice for Medicinal Products for Human and Veterinary Use2. The following year, EMA published two process validation guidelines11,12. These guidelines used a similar lifecycle approach to the one used by the FDA.The differences are mainly around terminology. For example,
- The early stage of product and process design are identified by the FDA as “Stage 1, Process Design,” whereas the EU refers to ICH Q89
- Stage 2 is called “Process Qualification (PQ)” by the FDA, whereas the EU document refers as “Qualification and Validation”1,2.
- In Stage 2, commissioning is included as part of the early activities (i.e., the “C” in “C&Q”). The term “commissioning” is not explicitly referenced in the EU document1,2.
- FDA uses the term “qualification” whereas the EU document talks in more granular terms by referring to IQ, OQ, and PQ1,2.
- What the FDA calls “PPQ” the EU documents still refer to this as “Process Validation” 9,10.
- Stage 3 is called “Continued Process Verification” (CPV) by the FDA, whereas the EU documents refer to this as “Ongoing Process Verification” (OPV)1,2.
Combining them All: The CQV Operation Lifecycle Model
As proposed in the graphic below, a fully integrated CQV Operational Lifecycle Model is applied to the validation of FUSEP.
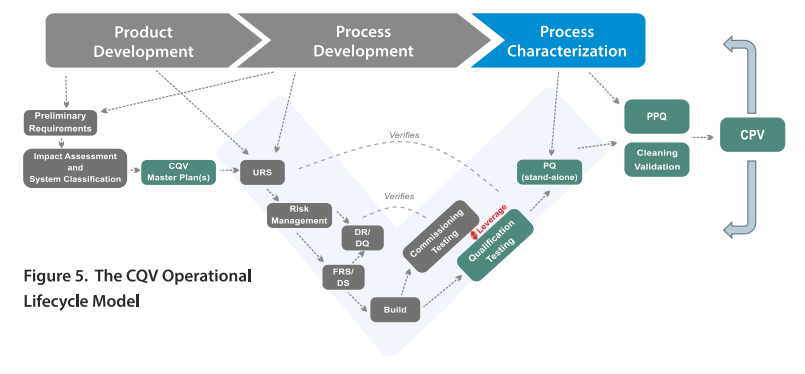 This model is different from all the other types of validation. From a CQV planning and project management perspective, the total number of deliverables in a CQV project for a new pharmaceutical/biopharmaceutical facility housing DS and/or DP operations should be divided into five main groups or workstreams (blue squares in Fig. 6).
This model is different from all the other types of validation. From a CQV planning and project management perspective, the total number of deliverables in a CQV project for a new pharmaceutical/biopharmaceutical facility housing DS and/or DP operations should be divided into five main groups or workstreams (blue squares in Fig. 6).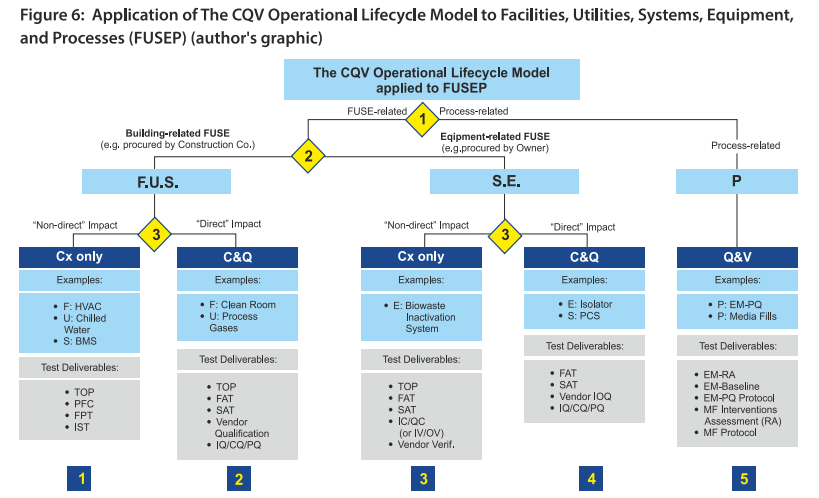
The CQV Operational Lifecycle Model can be applied directly to a new biopharmaceutical facility housing both DS and DP operations. There are three distinct decision points based on the following criteria (yellow diamonds in Fig. 6):
- Decision Point #1: Testing and Release of facilities, utilities, systems, and equipment (FUSE) vs. performance and PPQ testing.
- Decision Point #2: Testing and release of FUSE systems needed for the start-up and mechanical completion of the facility, usually procured by the construction (building) company vs. equipment and systems procured by the Owner, where qualification may be completed after mechanical completion.
- Decision Point #3: Extent of testing (i.e., commissioning-only vs. commissioning and qualification) based on impact on product quality (Direct vs non-direct).
Guiding the CQV program
An all-encompassing integrated CQV model can guide the CQV program in all possible scenarios, whether during the start-up of a new or modified facility or during the performance qualification and continued verification stages.
While my experience has found that choosing the right validation model can be a complex endeavor, every department within an organization should work toward this objective. Once a static process, validation has evolved to become a more dynamic process as pharmaceutical companies seek to simplify the validation process.
Companies can conduct a risk assessment on their facilities, utilities, and equipment to identify whether they impact processes or products.
References
- Food and Drug Administration. Guidance for Industry Process Validation: General Principles and Practices. Food and Drug Administration; 2011. https://www.fda.gov/files/drugs/published/Process-Validation–General-Principles-and-Practices.pdf
- European Commission. EU Guidelines for Good Manufacturing Practice for Medicinal Products for Human and Veterinary Use Annex 15: Qualification and Validation; 2015. https://health.ec.europa.eu/system/files/2016-11/2015-10_annex15_0.pdf
- International Society for Pharmaceutical Engineering. GAMP Guide. International Society for Pharmaceutical Engineering; 1994.
- Blackburn T. A Practical Approach to Commissioning and Qualification – A Symbiotic Relationship. Pharmaceutical Engineering. 2004;24(4). https://ispe.org/pharmaceutical-engineering/july-august-2004
- ASTM International. ASTM E2500: Specification, Design, and Verification of Pharma/Biopharma Manufacturing Systems and Equipment. ASTM International; 2013.
- International Society for Pharmaceutical Engineering. Baseline Guide Vol 5: Commissioning & Qualification 2nd Edition. International Society for Pharmaceutical Engineering; 2019.
- International Society for Pharmaceutical Engineering. Baseline Guide Vol 5: Commissioning & Qualification 2nd Edition. International Society for Pharmaceutical Engineering; 2001.
- International Conference on Harmonization. Quality Risk Management Q9. International Conference on Harmonization; 2005. https://database.ich.org/sites/default/files/Q9_Guideline.pdf
- International Conference on Harmonization. Pharmaceutical Development Q8(R2). International Conference on Harmonization; 2009. https://database.ich.org/sites/default/files/Q9_Guideline.pdf
- Food and Drug Administration. Pharmaceutical CGMPS for the 21st Century—a Risk-Based Approach. Food and Drug Administration; 2004. https://www.fda.gov/media/77391/download
- European Medicines Agency. Guideline on Process Validation for Finished Products – Information and Data to Be Provided in Regulatory Submissions. European Medicines Agency; 2016.
https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-process-validation-finished-products-information-data-be-provided-regulatory-submissions_en.pdf - European Medicines Agency. Guideline on Process Validation for the Manufacture of Biotechnology-Derived Active Substances and Data to Be Provided in the Regulatory Submission. European Medicines Agency; 2016.
https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-process-validation-manufacture-biotechnology-derived-active-substances-data-be-provided_en.pdf
Gerardo Gomez, Ph.D.
Director QMC-USA and CQV SME, PharmaLex
1 West 1st Avenue, Conshohocken, PA 19428 United States
Phone: (787) 356 – 4121, Email: gerardo.gomez@pharmalex.com
 Dr. Gerardo Gomez has more than 25 years of experience in the Pharmaceutical and Biotechnology industries. He has held technical and leadership roles in the areas of validations, technical transfer, operations, and regulatory compliance in major biopharmaceutical companies. He has been part of the Pharma Lex leadership team for the last 11years, conducting both strategic and tactical (execution) projects, while playing key roles for Pharma Lex clients- big and small – and for Pharmalex talent and business development initiatives. Gerardo earned his Ph.D. in Pharmaceutical Sciences from the University of Michigan, after graduating magna cum laude from the Chemical Engineering department atThe University of Puerto Rico.
Dr. Gerardo Gomez has more than 25 years of experience in the Pharmaceutical and Biotechnology industries. He has held technical and leadership roles in the areas of validations, technical transfer, operations, and regulatory compliance in major biopharmaceutical companies. He has been part of the Pharma Lex leadership team for the last 11years, conducting both strategic and tactical (execution) projects, while playing key roles for Pharma Lex clients- big and small – and for Pharmalex talent and business development initiatives. Gerardo earned his Ph.D. in Pharmaceutical Sciences from the University of Michigan, after graduating magna cum laude from the Chemical Engineering department atThe University of Puerto Rico.
Exclusives
by Gerardo Gomez
Director QMC-USA and CQV SME, PharmaLex
An article for Digital transformation is the process of using digital technologies to create new or modify existing business processes – By Satish Desai






